- Up to 50% of people with Parkinson’s disease will suffer from depression and up to 40% will suffer from anxiety.
- Despite the prevalence of mental health issues among people with Parkinson’s disease, only 2% are referred to mental health professionals.
- Mental health is as important as physical health for people with Parkinson’s disease.
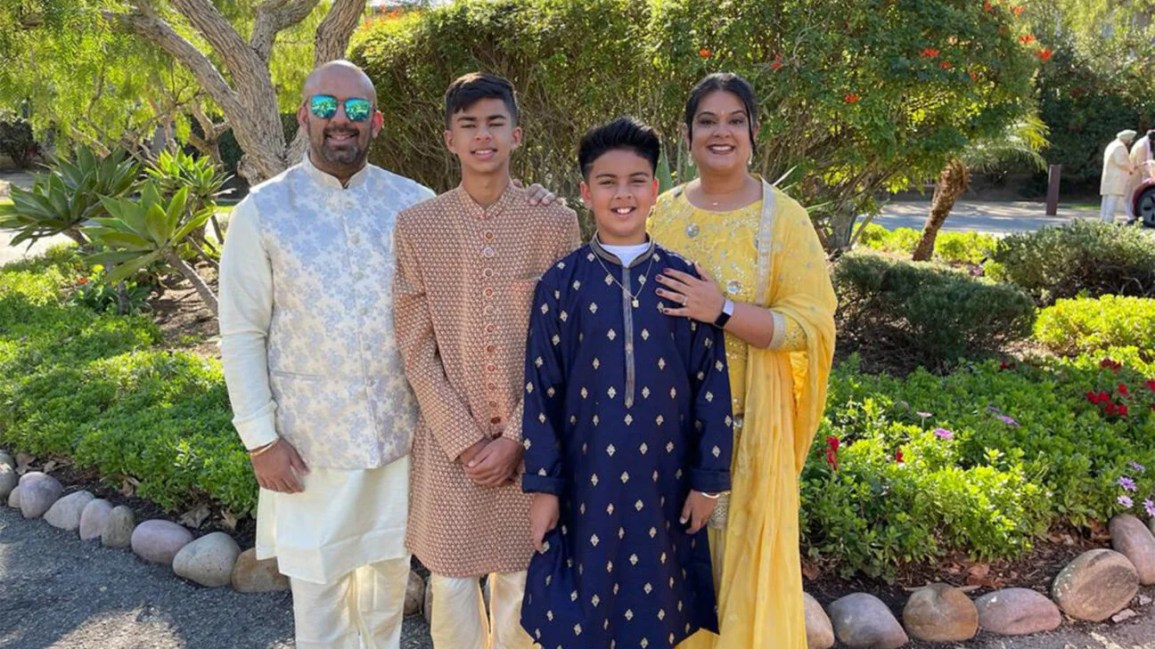
When Vikas Channin found out he had
“I could explain the depression and apathy I was feeling and hopefully combat those things with medication, exercise and diet,” he told Healthline.
A few years before his diagnosis, Channin began experiencing physical symptoms characteristic of Parkinson’s disease, including prolonged stiffness and pain in his legs that made walking difficult.
In 2021, he started having tremors in his right arm. After seeing doctors over the next few months, a DaTscan showed he had Parkinson’s disease.
Along with the physical symptoms, the diagnosis explained the cognitive impairments and mental health symptoms he was experiencing in the years leading up to 2022.
“(I) wasn’t as articulate as I was in the past…and there was a level of depression and withdrawal and a lot of that I attributed to the mobility issues I had,” Channin said.
For example, he stopped going to lunch with co-workers because he was worried he wouldn’t be able to keep up with them during the two-block walk. He also withdrew from social activities outside of work.
“When my wife asked me if I wanted to invite friends, I said, ‘Absolutely’. Who should we have more? but my answer became: ‘If you want, that’s fine with me, but I’m indifferent,'” a Channin said.
He attributed his feelings of depression and withdrawal to fatigue from coping with the physical symptoms he was experiencing, not knowing what was causing them, and to numerous visits to doctors and physiotherapists in the hope of finding relief.
Although he began seeing a therapist about a year before his diagnosis, it wasn’t until he was diagnosed with Parkinson’s disease that he learned of the disease’s connection to apathy (feeling indifferent or uninterested) and mental health issues such as anxiety and depression.
According to the Parkinson’s Foundation, up to 50% of people with Parkinson’s disease will suffer from depression, up to 40% from anxiety and about 40% from apathy.
The Parkinson Foundation says mental health issues are not just a reaction to being diagnosed with Parkinson’s disease, but rather part of the disease itself, caused by changes in brain chemistry.
Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital, said it makes sense given the neurotransmitters involved in Parkinson’s disease, depressive disorders and anxiety disorders.
“Each has a common origin, from which come the comorbidities of (Parkinson’s disease), depression and anxiety. It is understood that as dopaminergic pathways degenerate, an imbalance between acetylcholine and dopamine leads to Parkinson’s disease,” Torres-Mackie told Healthline.
The involuntary movements unique to Parkinson’s disease are usually the result of low levels of dopamine in the brain, she added.
“This neurotransmitter plays an important role not only in movement and coordination, but also in mood. Low levels of dopamine are also present in patients with depressive and anxiety disorders. Thus, as dopamine levels decrease, an individual may experience depressive and/or anxiety symptoms before or in conjunction with the diagnosis of Parkinson’s disease,” Torres-Mackie said.
In fact, she noted that depression, anxiety or apathy are often the first signs of the disease, with mood symptoms appearing earlier than other Parkinson’s symptoms.
“Specifically, we know from research that some people experience anxiety or depression 2 to 5 years before they are diagnosed with Parkinson’s disease,” she said.
However, data from the Parkinson’s Foundation Parkinson’s Outcomes Project showed only a 2% referral rate to mental health professionals, as well as potential underdiagnosis and undertreatment of anxiety and mental illness. depression in people with Parkinson’s disease.
Elena Godfrey, a registered clinical social worker for the Parkinson’s Foundation, said that historically good Parkinson’s care meant the best possible management of motor symptoms.
“Fortunately, people with Parkinson’s have added their voices to the conversation and are redefining what it means to get good care for Parkinson’s disease,” she told Healthline. “We now know that the non-movement symptoms of Parkinson’s disease have the greatest impact on a person’s quality of life, so good care for Parkinson’s disease must include assessment, discussion and treatment of non-movement symptoms, as well as general well-being.”
All facets of Parkinson’s should be considered by providers, as well as family and friends of people with the disease, Torres-Mackie said.
“Understanding the mental health ramifications of (Parkinson’s disease) can go a long way in increasing the ability of people with a diagnosis of (Parkinson’s disease) to live full and satisfying lives,” she said. .
Two weeks before Channin was diagnosed with Parkinson’s disease, he began taking antidepressants under the supervision of his therapist.
“Between the antidepressants, the response of a diagnosis, and the Parkinson’s disease medication, I was in a much better position after the diagnosis than before the diagnosis,” he said.
Taking care of your mental health requires as much attention as taking care of your physical health.
“Mental health is a constant battle and it’s really easy with Parkinson’s to let your world close in on you. There are dangers around every corner, there are places you can fall or trip over, problems with urinary frequency and urgency that make you dread being on the subway or at a concert. There are times when you feel like you might need some extra help when the meds aren’t working so well,” Channin said.
He continues to see a therapist regularly to help him cope.
He also turns to the following five key strategies to self-manage his physical and mental symptoms.
- Compliance with prescribed medications
- Eat healthy
- Exercise, such as cycling and rock steady boxing
- Prioritize good sleep hygiene
- Practice stress reduction
He also finds it comforting to speak on behalf of others with Parkinson’s disease.
“In my case, bringing people into my world was my way of fighting against this closing world. I embarked on a campaign to let people know what I was dealing with,” Channin said.
A representative from the Parkinson’s Foundation visited one of his boxing classes to talk about a fundraiser. Channin felt his participation was an opportunity to share his diagnosis with family and friends.
“I started to build a support network and people wishing me well and that helped my world not to close down and those around me started checking on me and asking me to get out of the house and go. meet me and get some fresh air and it’s been great for my mental well-being,” he said.
He wanted to pass on the support he had received to others, so he moved from working as an executive at a software technology company to doing outreach work in the Parkinson’s community.
“(It) seems like everyone has experienced before or after diagnosis, a level of depression and if you’re on the other side of that, which I like to think I am, you get that feeling of longing and urgently to help others. go out there and help them through the lean times,” Channin said.
Godfrey said people can live well mentally with Parkinson’s disease, but it takes effort.
“We rarely drift into mental and emotional health; it’s something we have to be intentional about, and living well with a progressive and chronic disease requires strong coping skills, prioritization and self-care,” she said.
Basic self-care concepts like getting quality sleep, eating healthy, exercising, and reducing stress are all important, as is staying socially active.
“It’s so important to engage in the thoughts and activities that give meaning and purpose to your life. With Parkinson’s, your energy is less and things take longer, so recognize that both of these resources (time and energy) are precious and spend them on the people and activities that matter most to you.” she declared.
If you’re on medication for mental health issues, it’s best to seek care from a psychiatrist who understands Parkinson’s disease or who is able to work with your neurologist, Godfrey added.
Additionally, turning to the following resources provided by the Parkinson’s Foundation may provide additional support:
- The Parkinson Foundation website includes expert briefings, podcasts, fact sheets, videos, webinars and more on the subject of mental health.
- The Parkinson’s Foundation Helpline (1-800-473-4636) welcomes calls from people with Parkinson’s disease, their families, friends and healthcare providers, and offers information about all aspects of Parkinson’s disease, including referrals to healthcare professionals and community resources for support.
- PD Conversations is a place to connect with others living with the disease.
“(There are many) ways to focus on your own mental health and well-being and the more options you have and the more resources you consider, the more likely you are to figure out what works for you,” said said Godfrey.

