CNN
—
U.S. health officials released a final rule that not only makes some changes to Medicare — including expanding access to behavioral health care and clarifying criteria guidelines — but cracks down on ads.” misleading”.
On Wednesday, the US Department of Health and Human Services, through the Centers for Medicare and Medicaid Services, finalized the rule which, among other things, prohibits advertisements that do not mention a specific plan name and use the logos or Medicare language in a manner that could mislead and confuse enrollees into believing that the advertisements are from the government.
The moves are the latest in efforts by the Biden administration to curb Medicare Advantage plans, which have grown in popularity. About half of Medicare participants are enrolled in these plans, which are managed by insurers under contract with the federal government.
According to CMS, the “proliferation of certain television advertisements” promoting enrollment in Medicare Advantage plans – which are offered by private Medicare-approved companies – is concerning.
“Today, we are announcing a rule that will crack down on deceptive marketing schemes by health insurance companies that offer Medicare Advantage plans, those that offer Part D prescription drug plans, and their downstream entities. provisions, the rule would prohibit overbroad advertisements about the Medicare Advantage program that often tend to confuse and mislead those eligible to enroll in some of these insurance plans,” HHS Secretary Xavier Becerra said Wednesday. .
Overall, about 65 million Americans participate in Medicare, according to Becerra.
“Any marketing that doesn’t specifically name a health plan, that misrepresents what a plan might offer in those ads, is something that would now be banned,” he said. “This is going to be important because the confusion that often arises and the changes that some enrollees will often make to their detriment to get health care are things we want to try to avoid.”
Last year, the Senate Finance Committee released a report highlighting an increase in these deceptive marketing practices that target seniors with Medicare Advantage plans and recommending that CMS take steps to reduce the prevalence of these marketing tactics.
“We’ve heard from many seniors and people with disabilities about misleading and confusing advertising for Medicare Advantage and Part D plans. Today’s final rule includes changes to protect people exploring Medicare Advantage and health coverage. Part D Against Confusing and Potentially Deceptive Marketing Practices,” Dr. Meena Seshamani, CMS Deputy Administrator and Center for Medicare Director, said Wednesday. “We are finalizing 21 marketing provisions to protect beneficiaries.”
Beyond marketing requirements, the final rule clarifies criteria guidelines to help ensure people with Medicare Advantage receive the same “medically necessary” care they would receive with traditional Medicare.
The rule also expands the list of populations to which Medicare Advantage organizations must provide “culturally competent” services, such as people with limited English proficiency or those in the LGBTQ community. Additionally, the rule requires that a pre-authorization approval for care remain valid for as long as “medically necessary” to avoid interruptions in care for recipients.
“We are also finalizing new minimum wait time standards for behavioral health,” Seshamani said, while requiring that most types of Medicare Advantage plans include behavioral health services.
The American Hospital Association said in a statement Wednesday that it applauds the increased attention to Advantage plans.
“Hospitals and health care systems have sounded the alarm that beneficiaries enrolled in certain Medicare Advantage plans routinely experience inappropriate delays and denials of coverage for medically necessary care,” said Ashley Thompson, vice president. senior president of the group for the analysis and development of public policies. “This rule will go a long way to protecting patients and ensuring timely access to care, as well as reducing inappropriate administrative burden on an already overburdened healthcare workforce.”
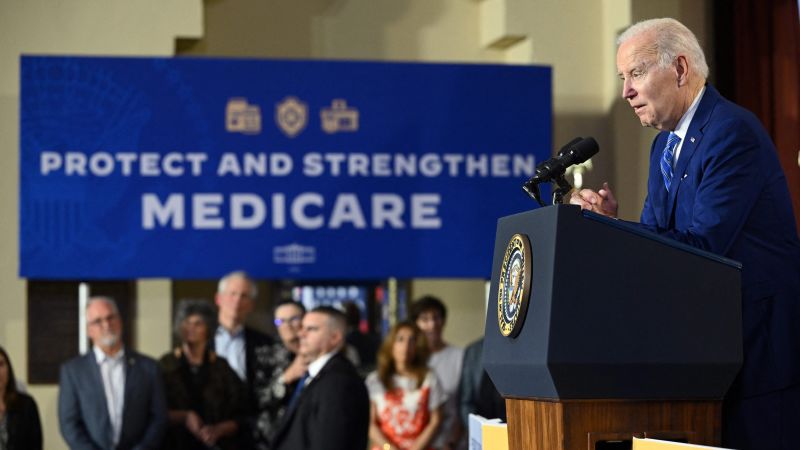
Protecting and strengthening Medicare is a top administration priority, CMS Administrator Chiquita Brooks-LaSure said in a press release Wednesday. “With this final rule, CMS is implementing new safeguards that make it easier for people with Medicare to access the benefits and services to which they are entitled, while strengthening the Medicare Advantage and Part D programs.”
On Friday, CMS issued controversial final payment policies for 2024 that aim to limit overbilling by Medicare Advantage plans. Changes include updating the risk adjustment model to better ensure that payments are consistent with patients’ medical conditions and that insurers are not adding diagnoses to inflate their billing.
Insurers vehemently protested the proposed rule, leading CMS to spread the changes over three years, instead of one.